Engaging your patients while executing different pieces of the revenue cycle is challenging yet extremely essential. Read on to learn about the elements of your revenue cycle that require patient participation, along with some suggestions that will help improve their experience as they delve deeper into complex administrative processes related to the care lifecycle.
A robust revenue cycle provides a consistent supply of fuel through seamless financial transactions ensuring the optimal functioning of a healthcare establishment. Any interaction between patients and their physicians or utilization of facilities provided by the entity generates a cost that needs to be reviewed and billed appropriately to either third-party payors or the patients themselves. Smooth operations in this area are, therefore, of utmost importance when it comes to long-term sustenance of a healthcare unit of any size. A patient’s involvement in the revenue cycle is inevitable and requires greater attention as it adds to the patient’s overall experience.
A patient’s passage through the revenue cycle can be broken down into the following major blocks:
1. Pre-Registration
When a patient walks into your facility for the first time, it is critical to collect as much information as possible, especially concerning their insurance enrollment. Such advance preparation helps in avoiding payment-related chaos after the services are rendered. It is also an excellent idea to give the patient a walkthrough of the administrative aspects that would require their input as well as a list of documentation that they need to keep handy.
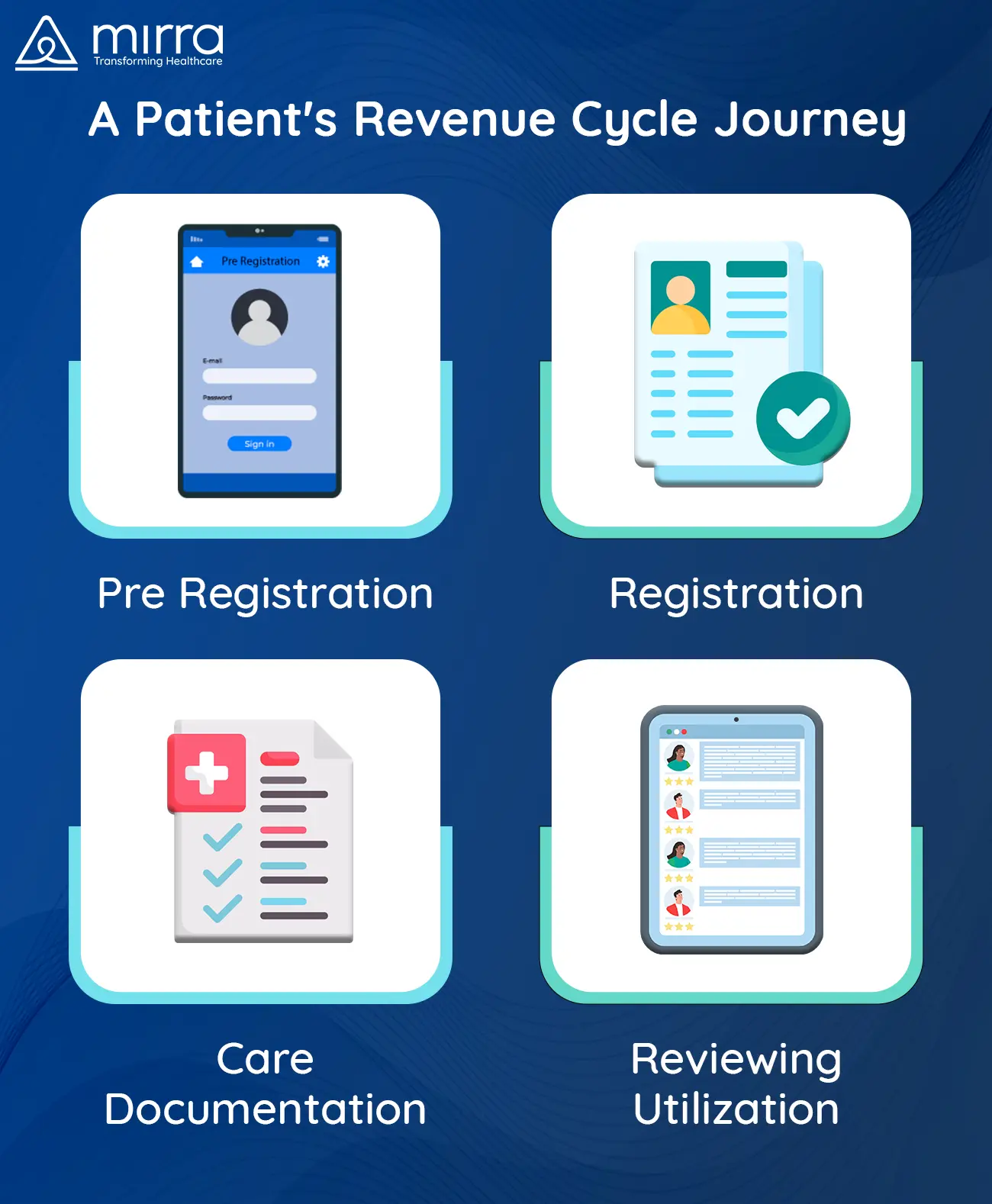
2. Registration
By this time the administrative staff is equipped with all the necessary details of the patient’s payment options and can, therefore, alert them with regards to the potential financial implications of their treatment as well as brief them about the steps that will follow. Such a high degree of transparency embeds confidence in the patients, making them believe that they are in the right hands.
3. Documentation of Care
Once the treatment begins, it is crucial for physicians to keep an adequate and precise record of all the clinical services provided. Accurate documentation helps in ensuring flawless billing. Although patients are not directly involved in this process, it is still vital for the staff to make sure that they understand the treatment protocols.
4. Reviewing Utilization
Case Managers step in at this stage to evaluate the treatment protocols and check the progress of the patient. These specialists carefully inspect the quality of care as well as the requirement of the prescribed services, to highlight unnecessary fragments, if any. Patients are an essential part of this process as the Case Managers will seek their input before chalking out a plan.
Read more: How Case Managers Can Help Reduce Healthcare Costs
5. Coding
While patients are not a direct part of this process either, the codes that are assigned by qualified medical coders to the services incurred as part of the treatment, find a place in their health records. Even though these codes may make no sense to them, they add up to the final cost of treatment and, therefore, directly affect the patients.
6. Pursuing Third-Party Payors
It is the prerogative of the healthcare unit to pursue payors that are liable to pay on behalf of the patients. This process needs to be done diligently and tirelessly to make sure that patients are not handed an unreasonably inflated bill. This process includes the creation and submission of claims that are error-free so that they go through without any iterations.
7. Figuring Out Patient Responsibility
After the payments have come through from the third-party payers, the remaining charge has to be borne by the patient. This phase is where patients need maximum assistance since they may not understand the breakup of costs, or what other options they can explore, before paying the entire amount.

If your establishment can offload the patient’s burden by making them more aware of the nitty-gritty associated with the financial aspect of their treatment, you are bound to leave an indelible impression on them. With the support of this kind, patients will find themselves in a better position to make decisions and prepare for the future. Mirra Health Care (TPA), a healthcare management company, can help you design your revenue cycle management processes in such a way that the patient is always at the epicenter of all decisions and activities, elevating your patient engagement score infinitely.
For more information on how you can partner with Mirra and utilize the services in their Medicare in a Box solution, get in touch with our experts to book a demo.