Credential Verification is complicated and involves copious amounts of paperwork. Despite the financial and mental burden that it imposes on healthcare entities all over the country, there is no way around it as it is a legal mandate that ensures that only qualified and competent physicians are allowed to provide care. It is possible to make life easier though by following a set of simple guidelines.

When it comes to credentialing, most administrative departments at healthcare entities – big or small – start hyperventilating. There is a good reason behind this extreme reaction. The sheer magnitude of work involved in verifying new physician’s credentials is terrifying to say the very least. Due to the labor-intensive nature of this task, it usually gets pushed to the last minute. It is, therefore, not surprising that credentialing-related paperwork is often haphazardly put together or that there are several instances of late submission. These mistakes hamper not just the fiscal health or your organisation, but also cause significant inconvenience to patients who are pre-scheduled to meet a physician whose credentials are yet to be verified. To avoid nightmarish eventualities like the ones mentioned above, it is imperative to keep a set of 5 guidelines in mind while working towards getting one of your physicians credentialed. These rules are as follows:
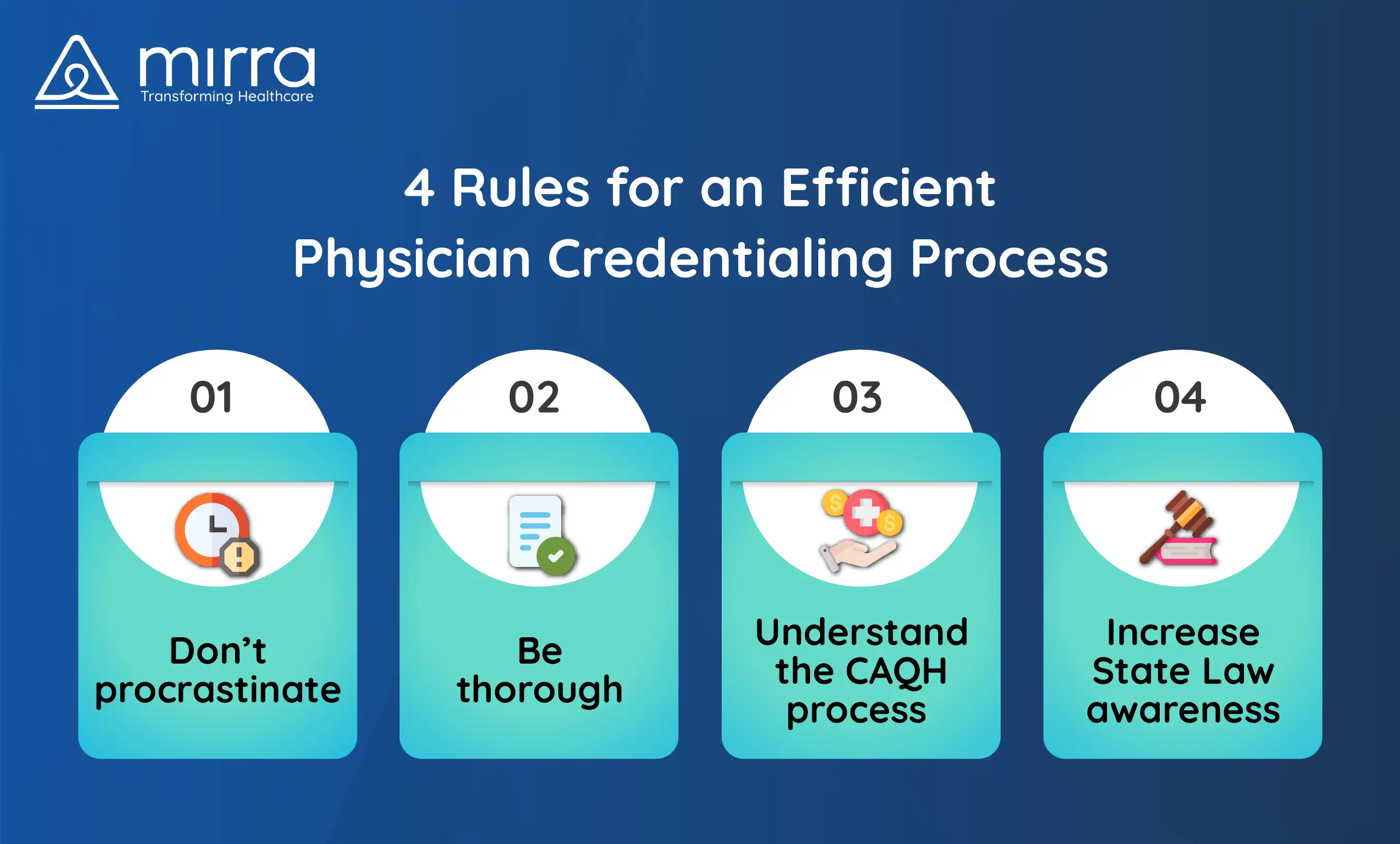
Don't Procrastinate
Starting the credentialing process right away, or if possible even before a new physician shows up to work, is a great practice. Such eagerness will not just help complete the process in an organised manner, but will also reduce the frustrating gap during which doctors can’t do much but twiddle their thumbs as they wait to finally be able to start seeing patients. Most payors claim to take no more than 90 days, but factoring in errors and resubmissions it may take anywhere up to 150 days for the process to be done and dusted.
Be Thorough
As much as 85% of the documentation submitted is incomplete or carries invalid information, as per a leading insurance provider. The areas that contain the maximum amount of discrepancies include employment details, malpractice history, insurance information, information regarding hospital privileges, and attestations. Knowing what needs to be submitted and making sure that everything needed is collected and dispatched on time is pivotal when it comes to flawlessly completing the process.
Read more: 4 Challenges That Make Physician Credentialing A Tough Task | Mirra HCUnderstand the CAQH process
CAQH or Coalition for Affordable Quality Healthcare is an entity that offers a uniform credentialing system that is adopted by most payors. If you ensure that your physicians’ latest credentials are up to date with CAQH, then the entire credentialing and re-credentialing cycle becomes smoother and quicker.Increase Your Awareness Regarding State Laws
Many states have independent requirements for credentialing. By keeping abreast with all the state-specific nuances, you can avoid unnecessary or duplicate paperwork. For instance, some states have an ‘in-state credentialing’ clause that states that if a physician is shifting to another employer within the same state, their credentials need not be verified again as long as their latest employment information is updated.
Credentialing can be a dreary process but it can be made simpler by being meticulous and following the rules listed above. Partner with a trusted TPA like Mirra Health Care to zap your credentialing woes forever.
For more information on how you can partner with Mirra and utilize the services in their Medicare in a Box solution, get in touch with us