Denial Management is an area that not just needs greater focus but also a more organized and professional approach, now more than ever. Read on to learn about the circumstances that plague the healthcare industry today and how they create an urgent need for a magnifying-glass approach towards identifying and ironing out the faults that cause practices and hospitals to bleed financially.
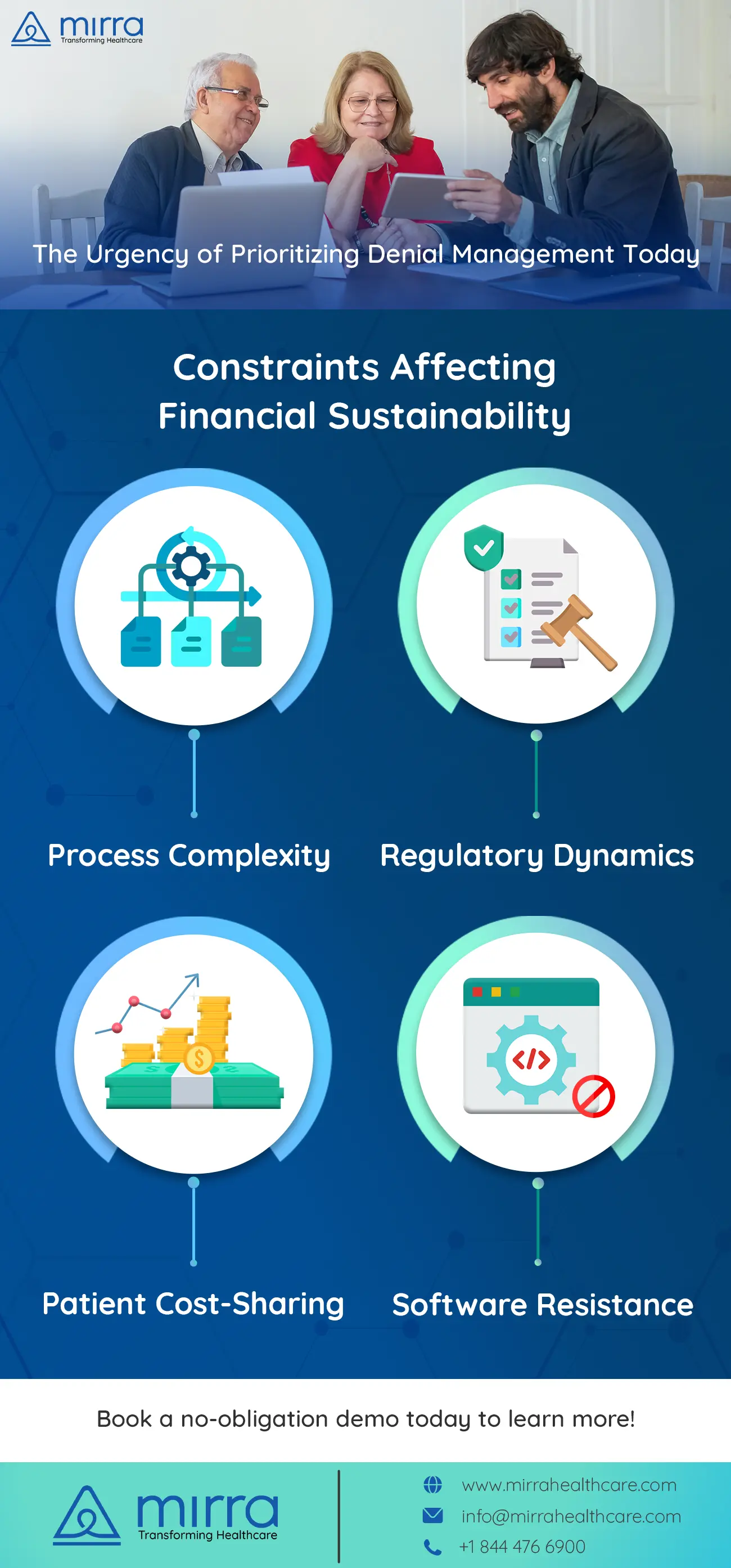
Like any other business enterprise, healthcare entities also require sound fiscal health to thrive. Well-planned self-improvement initiatives, meticulous programs to enhance the patient experience, and investments in cutting-edge technology and research are all elements that make a healthcare entity a cut above the rest. Unfortunately, the world of healthcare is riddled with external factors that pose a threat to the inflow of cash that can be used to promote these advancements. Some of these factors are as follows:

1. Process Complexity is Higher Than Ever Before
With insurance companies adding new-fangled clauses into contracts making them even more intricate and difficult to adhere to fully, the percentage of claims denial is on the rise. A majority of claims submitted are usually denied in the first go and require a considerable amount of rework to be sent back and accepted.

2. Frequent Changes In Regulations
In the past few years, there has been an onslaught of modifications in mandatory regulations when it comes to the coding and billing part of the claims preparation process. Fledgeling practices and well-established hospitals both have a hard time keeping pace with these frequent legal changes, and this adds to the reason behind the denial of claims.
3. Higher Patient Responsibility
High Deductible health insurance options have gained popularity amongst employers. Such plans hike up the patient’s portion of the overall payment that the provider is entitled to get. Settling bills directly with patients is way more difficult than getting paid directly by a government agency or an insurance provider.
4. Hesitance In Switching to A Denials Management Software
Many healthcare facilities still believe in a manual denial management process. Manual management of denials is quite inefficient in light of all the complications that shroud the claims management process. Switching to a sophisticated automated tool that eliminates errors in the information being submitted as well as takes care of timely submission of claims can bring down the denial rate considerably.

Mirra Healthcare, a TPA , instituted by physicians, boasts of experienced, hands-on professionals who have in-depth knowledge in the field of Denial Management. By getting Mirra onboard as a consulting entity, you can get full-fledged support in redesigning your Denial Management processes so that you are well prepared for handling the external factors that are likely to weaken your practice’s financial condition. You can also opt to outsource your entire Denial Management package to Mirra and entirely focus on patient care without worrying about revenue flow. For more information on how you can partner with Mirra and utilize the services in their Medicare in a Box solution, get in touch with us and book a demo.