The escalating rate of claim denials is causing ripples throughout the healthcare landscape, presenting a formidable challenge for providers. This issue affects operational efficiency and directly impacts the quality of the patient care management system and business performance.
In this blog post, we examine the complexities that come with real-time adjudication challenges and offer strategic insights for its effective mitigation. We will also share how Mirra's Claim Adjudication solution can easily handle claim denial complexities, ensuring seamless operations and enhanced patient outcomes by streamlining the claims adjudication process. Let's get started.
Understanding Claim Denials
Claim denials in healthcare denote an insurance company's refusal to pay a healthcare provider's request.
According to research, claims processing was identified as the second-largest contributor to "wasted" healthcare dollars in the US, amounting to an estimated $210 billion in 2009, which soared to $265 billion by 2019. This data, sourced from a pre-pandemic American Hospital Association (AHA) survey, further highlighted a substantial increase in denials. Additionally, 89% of hospitals and health systems reported a rise in denials over the preceding three years, with half describing the surge as "significant."
Post-pandemic, Experian Health data highlighted a 10% to 15% increase in denials, with 70% of responders recognizing the importance of claims management. A significant 52% have upgraded their claims processing tech, signaling their importance to technology-driven healthcare success.
The data calls for innovative solutions and proactive measures to ease the mounting pressure on healthcare organizations.
Introducing Mirra's Claim Adjudication Solution
Overview
- Holistic Approach: Mirra's Claims Adjudication Solution offers a comprehensive approach to transform claims management.
- Integrated Functionality: It seamlessly converts paper claims into digital records, processes electronic claims, and maintains a centralized payment reimbursement system.
How Mirra's Solution Tackles Claim Denials
Now, Mirra's TPA Claims Adjudication solution can help prevent claim denials in the first place through its following features:
- Automated Processing: Mirra's solution is highly automated, reducing errors by ensuring claims are thoroughly reviewed before submission.
- Real-time Error Detection: The system promptly identifies discrepancies, facilitating quicker issue resolution and error-free operations.
- Enhanced Communication: Streamlined communication and reporting mechanisms optimize the claims management process.
- Versatility: Mirra's solution integrates seamlessly with third-party gateways, offering adaptability through products like ClaimsLite® and ClaiMaster® for diverse CMS- mandated claims.
- Advanced Editing Software: Equipped with over 40 million edits, including CMS NCCI edits, this software ensures compliance and reduces the likelihood of fraudulent claims.
- Applicability: Mirra's solution caters to various healthcare plans (HMOs, PPOs, Dental, Vision, etc.), emphasizing timely and accurate claims processing, aligning with evolving industry needs.
Read more: Improve Revenue Cycle Management in Healthcare| Mirra HC
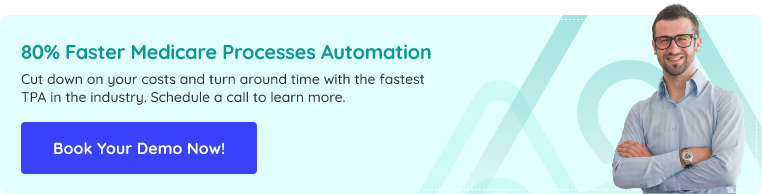
Root Causes of Claim Denials
Understanding the fundamental causes behind claim denials is crucial in devising effective strategies to mitigate their impact. Several vital reasons contribute to claim denials within the healthcare system:
A. Inaccurate or Incomplete Information in Claims
Insufficient data or inaccuracies within submitted claims often result in their denial. Missing or incorrectly filled-out fields, incomplete patient information, or errors in coding contribute significantly to this issue.
B. Coding Errors or Improper Documentation
Errors such as mismatched codes, upcoding, or insufficiently documented procedures lead to claim rejections. Accurate coding is vital for proper claim adjudication.
C. Insufficient or Improper Verification Processes
Lack of proper verification protocols or inadequate validation processes often lead to claim denials. Verification gaps in patient eligibility, coverage, or procedural requirements can result in claim rejection
D. Rejected Claims Due to Non-Compliance or Outdated Practices
Claims may be declined due to non-compliance with regulatory changes, outdated billing practices, or healthcare policy and guideline inconsistencies.
Mitigation Through Mirra's Claims Adjudication Solution
Mirra's TPA Claims Adjudication Solution significantly mitigates these root causes. By integrating advanced technologies like AI and machine learning, Mirra's solution ensures:
- Enhanced accuracy in claims submissions through automated validation and verification processes.
- Real-time error detection and correction, reducing coding errors and incomplete information.
- Improved compliance and adherence to evolving regulations reduce claim rejections due to outdated practices or non-compliance.
Learn about the 7 Benefits of Outsourcing your Medical Claims Management | Mirra HC
Impact of Claim Denials
Understanding the profound repercussions of claim denials within the healthcare ecosystem is crucial as it impacts various aspects of healthcare providers and patients alike:
A. Financial Strain on Healthcare Providers
Claim denials strain healthcare finances, causing revenue losses and hampering financial stability. This can affect investments in infrastructure, staff training, and patient care quality.
B. Patient Care Delays
Claim denials result in delays in essential patient care and treatments. Administrative processes to resolve denials consume valuable time, potentially impacting patient outcomes.
C. Increased Administrative Burden
Managing claim denials increases administrative workload and costs, reducing productivity and raising stress levels among healthcare professionals.
Implement it Easily
Implementing Mirra's solution is designed to be hassle-free, making the transition as smooth as possible and enabling you to realize benefits rapidly. Our seamless onboarding process includes:
A. Practical Steps for Healthcare Providers to Adopt Mirra's Solution
Simplified Assessment and Planning: Mirra's implementation begins with assessing your current claims adjudication process. This step identifies bottlenecks, inefficiencies, and areas for enhancement. This ensures a streamlined assessment, giving clear insights into areas needing immediate attention, making it a seamless experience.
Tailored Strategy and Objective Alignment: Upon understanding your current system's pain points, Mirra tailors a comprehensive strategy aligned with your objectives. This ensures a focused roadmap aligned with your health plan's success.
Seamless Integration with Existing Systems: The integration process is effortless, ensuring the solution integrates perfectly with your current systems without disrupting ongoing operations.
Learn More : Strategy to Reform Traditional Revenue Cycle Management in Healthcare | Mirra HC
B. Easy Integration with Hands-On Training
- Smooth Integration: Mirra's implementation team will collaborate with you closely to ensure a smooth integration process. They will establish clear communication channels and milestones to track progress. They will regularly review and address any integration-related issues that may arise during the process.
- Comprehensive Training Programs:Mirra's team will conduct comprehensive training sessions for all users, ensuring they have a deep understanding of the solution's functionalities. They will offer ongoing training and support to address any queries or challenges encountered.
- Monitoring and Continuous Improvement:A monitoring mechanism will be established to track the performance metrics post-implementation. It will analyze the collected data to identify areas for continuous improvement and optimization.
- Regular Updates: Mirra's solution will regularly update and fine-tune the system to adapt to evolving healthcare industry standards and regulations.
The Bottom Line
Proactive action is essential for mitigating claim denials and ensuring smooth revenue cycle management within healthcare businesses. Mirra's Claims Adjudication solution addresses the challenge of claim denials and helps ensure a future where healthcare organizations can operate efficiently, ensuring fiscal health and optimal patient care delivery. Reach out to our experts to book a demo today!