Utilization Management (UM) has become an indispensable piece of the overall management strategy at any healthcare entity today. Read on to learn about the elements that make up for a successful UM program and how such an initiative can help providers reduce their claims denial rate, provide on-point care, and minimize overall healthcare costs.
Most physicians view UM techniques with an exceptionally critical eye since they do not understand the total impact and long-term benefits of such interventions. What exacerbates this skepticism is the fact that, on the surface, the processes deployed as part of any UM initiative seem to curtail the clinical autonomy that they enjoyed in the past. Besides, the additional administrative burden generated by such a program does nothing to improve its acceptability or popularity amongst an already over-worked staff. To be able to thoroughly appreciate the advantages accrued by implementing an effective UM framework, it is critical first to understand the basics of UM.
A robust UM plan consists of three interlinked elements – utilization review, risk management, and quality assurance. Utilization review is the first step that aims at assessing the requirement and appropriateness of care provided. The results of utilization review feed into the other two pieces. Using these inputs, it is possible to design quality improvement and risk mitigation plans for future cases. Utilization review runs in three phases:
- Pre-treatment Review – Just before running any treatment protocols, the prescribed treatment plan is evaluated to verify its requirement and aptness.
- Concurrent Review – Reviews at fixed intervals during the treatment process are essential to nip any potential issues in the bud. Such evaluations check the soundness of care management activities like transition planning, care coordination, discharge planning, and post-discharge follow-up schedule.
- Post-Treatment Review – To gain insights that can prove valuable for quality management and risk assessment, it is important to study every case post-discharge. This analysis includes reviewing all the pending claims, checking the accuracy of the codes assigned, and tallying the reimbursements received with the claims filed to identify gaps.
In light of all the benefits of a well-planned UM intervention, CMS has made it mandatory for hospitals to implement such a plan to qualify for Medicaid or Medicare reimbursements. As a result, most hospitals and healthcare practices are running such programs. Some of the best practices followed by entities that have implemented fruitful UM programs are as follows:
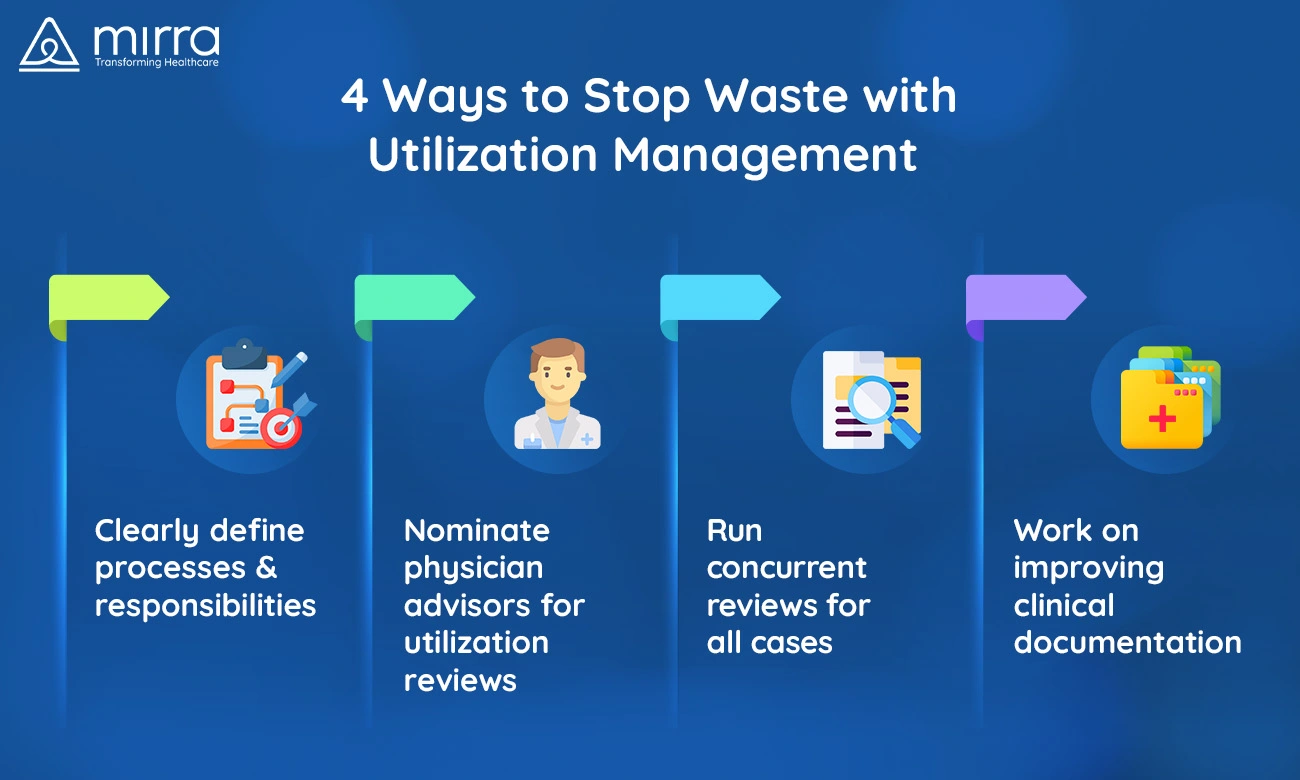
- Clearly Define Processes, Responsibilities, And Authorizations – A clearly outlined utilization review plan that defines each person’s responsibilities and authorities can go a long way in ensuring sustainability. Process documentation that includes guidelines for admissions, professional services, and care setting reviews is another step in the right direction.
- Nominate Dedicated Physician Advisors For Utilization Reviews – Physicians who also have specialized knowledge of healthcare policies, and revenue cycle processes can be roped in to act as a link between clinical and administrative staff while conducting utilization reviews. Such advisors are an asset to any UM initiative as they can look at the entire picture that includes clinical, financial, and legal aspects.
- Run Concurrent Reviews For All Cases – For all admitted patients, it is essential to run concurrent reviews as part of their care management plan. Consistent reviews will lead to the creation of backup documentation supporting all the services rendered. Paperwork of this kind makes it easier for you to appeal rejections and retrieve denied payments by proving medical necessity
- Work On Improving Clinical Documentation – While analyzing the results of utilization review, it is critical to spot clinical documentation errors and work out strategies that can prevent similar mistakes in the future. Such an approach isu beneficial in easing the job of utilization reviewers and payers and cutting down the chances of denial of claims.
If you too are looking to establish an excellent UM strategy for your venture, consider partnering with Mirra Health Care (TPA), a healthcare management setup that employs professionally qualified personnel who can help you not just draw up a great UM plan, but also run it with the diligence that is required to make such a project a success!
For more information on how you can partner with Mirra to utilize their Medicare in a Box service, get in touch with us today.












