Utilization Management (UM) has become a necessity in our healthcare landscape today especially since the focus has shifted towards avoiding indiscriminate use of healthcare resources. Read on to learn more about the concept of Utilization Management and the activities it encompasses.
Utilization Management is a practice that involves a set of activities that aim at containing costs without compromising the quality of care delivered to the patients. In a prosperous nation like the United States where the cost of health care has been steadily rising and has reached an exorbitant figure of over $10,000 per person per year, such cost-saving strategies are much needed. The establishment of value-based instead of service-oriented reimbursement philosophy is a step towards urging healthcare professionals to invest in UM strategies to improve both health as well as financial results.
Read more: Utilization Management's Impact on Healthcare Organizations | Mirra HC
Here are some important activities that form the framework of any successful UM program:
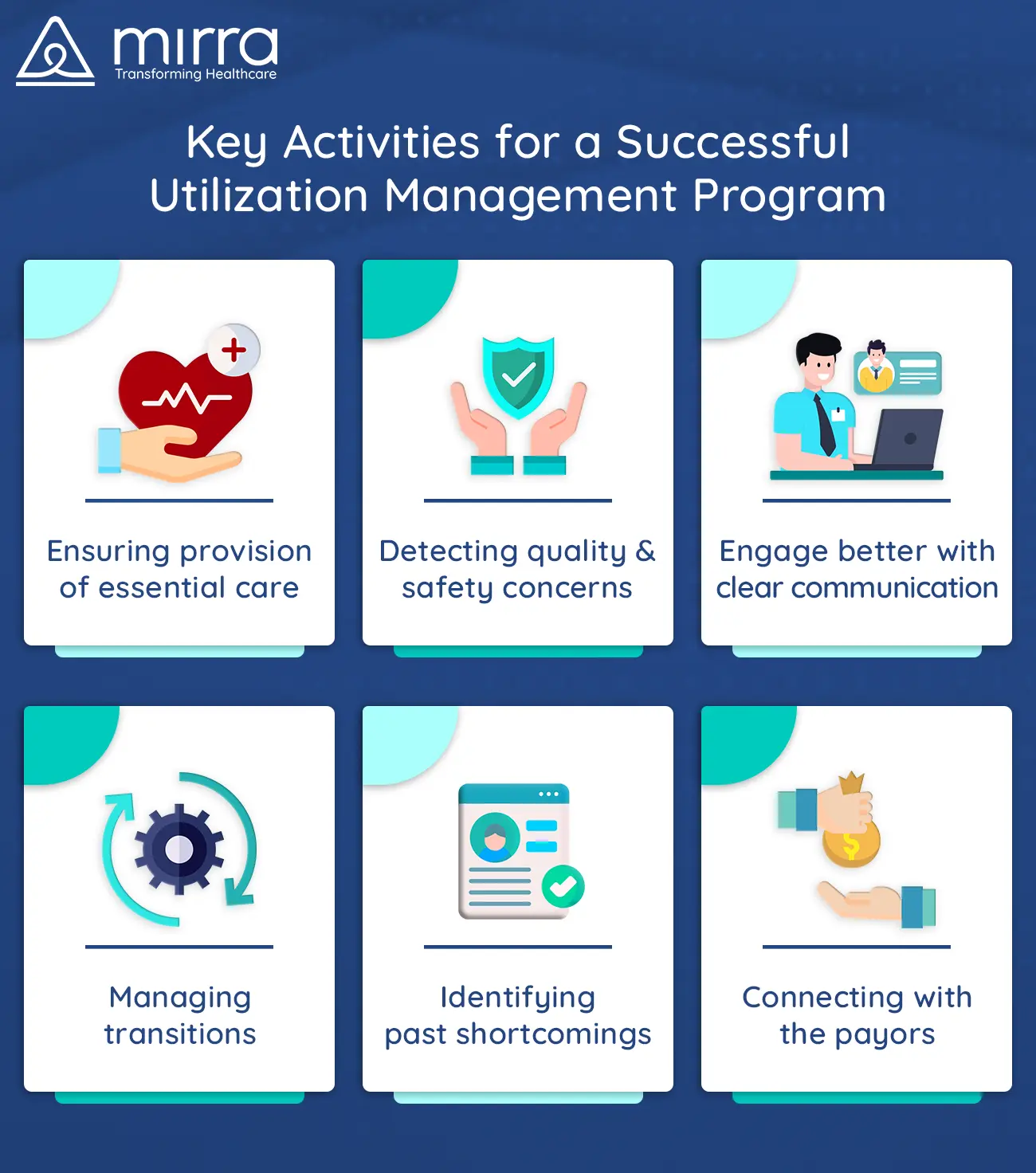
1. Ensuring Provision of Suitable and Essential Care
It is vital to ascertain the necessity and the effectiveness of care throughout the patient’s treatment lifecycle. Such periodic interventions help in avoiding costs that accumulate as a result of duplication of efforts, incorrect diagnosis, and unnecessary medications.
2. Detecting Quality and Safety Concerns
Any potential issues that sabotage the quality of treatment that a person is receiving as well as its safety are caught as part of the constant monitoring process. While screening a patient’s treatment, UM personnel keep in mind the patient’s health history and other facets of their socio-economic background too.
3. Enhancing Engagement Through Communication
One of the most critical features of a UM strategy is keeping patients connected to their healthcare support system. Educating them on how to manage their well-being even after they have left the premises of the healthcare facility, reminding them of follow-up appointments, and ensuring that they adapt to any changes in medication or dosage that their provider has recommended are some examples of how UM methods try improving the results.
4. Managing Transitions
During treatment, especially in the case of those who are chronically ill, transitions are bound to happen. This could either mean getting discharged and going home or moving to another specialized facility or even to an assisted living community. UM, specialists manage such transitions so that there is no disruption in care.
5. Identifying Past Shortcomings
By reviewing the documentation detailing the case history of a patient, UM personnel can zero in on the gaps in care provided so far. Using this information, providers can assess methods to avoid such failures in the future.
6. Connecting With The Payors
Another crucial aspect of the UM plan is to ensure insurance coverage and eligibility to avoid any confusion during the billing process. Frequent interaction with payor sources to stay abreast with any plan-specific agreements or changes in regulations is a best practice in the UM space.
Not all healthcare facilities are equipped with the necessary human resources as well as the knowledge that is needed to take on the responsibility of executing UM interventions. It is, therefore, a good idea to enlist the services of an organization that specializes in UM to keep both cost and quality in check. Mirra Healthcare (TPA) is one such organization that employs qualified UM professionals who are capable of swooping in and making a world of a positive difference to the way your organization operates. For more information on how you can partner with Mirra and utilize the services in their Medicare in a Box solution, get in touch with us today.












