Nearly 20%* of healthcare claims are denied due to avoidable issues, coding errors, incomplete documentation, and manual bottlenecks. That’s not just frustrating, it’s expensive. With denial rates posing a significant challenge in the claims process, there is a need for a swift and effective solution. Automation ensures precision and productivity while helping healthcare businesses navigate claims seamlessly, minimize errors, and significantly improve operational productivity.
And this is precisely what Mirra's Claims Adjudication Solution does. It's a strategic asset that addresses rising denial rates, drives operational excellence, and ensures consistent revenue streams.
In this blog post, we will share how automation acts as an essential component of the claims adjudication process for both payers and providers. So, let's get started. Read on.
Current Challenges in Healthcare Claims Management

The following are some of the most pressing challenges facing the healthcare claims management landscape:
1. Escalating Denial Rates: Denial rates typically range from 10% to 20% but can be as high as 40% in some cases, placing a heavy burden on revenue cycle management (RCM) teams and delaying revenue collection.
Also, read Expert Strategies to Stop Claims Processing Denials
2. Manual Processes' Limitations: Labor-intensive manual procedures result in errors, inefficiencies, and delays. These processes strain resources and disrupt revenue cycles.
3. Stringent Regulatory Requirements: Keeping up with evolving national and international regulatory standards, such as NPHIES and Minimum Data Set (MDS) requirements is complex. This can result in non-compliance risks such as financial penalties, claim denials, and reputational damage.
4. Data Discrepancies: Many healthcare organizations lack access to real-time analytics on claims performance, payer trends, and compliance gaps. This limits proactive issue resolution and financial optimization. Disconnected data sources and formats hinder seamless integration, leading to inaccuracies in TPA claims submissions.
These challenges significantly impact operations and profitability.
Read more: How to Boost Your Healthcare Revenue Cycle | Mirra HC
Understanding Mirra's Automated Claims Adjudication Solution

Mirra's Claims Adjudication Solution is an advanced system designed to streamline and digitize the healthcare claims management process. It offers capabilities that facilitate easy transitions from paper-based claims to digital records while efficiently handling electronic claims. This robust solution is a comprehensive all-in-one reimbursement system, ensuring swift and accurate payment processing.
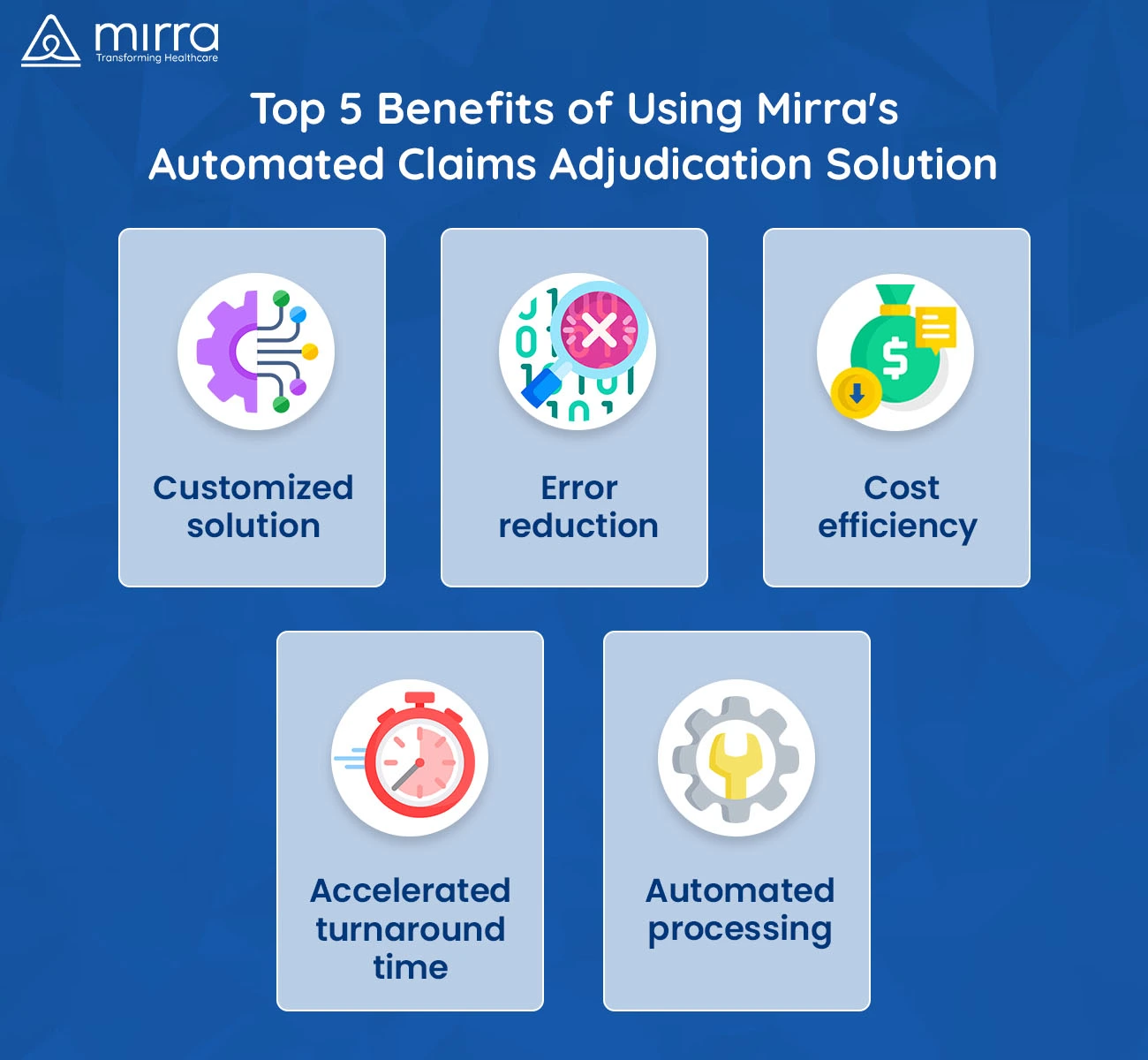
Key Benefits
For Payers:
-
Customized Solution: Mirra's solution is tailored for easy integration and handling, offering customized settings aligned with distinct healthcare provider requirements. Whether it's HMO, PPO, Dental, or Vision, the solution adjusts to your plan's unique needs.
Also, read Why Custom Claims Adjudication Software Works Better
-
Error Reduction: The system significantly minimizes errors compared to manual intervention, ensuring precise and reliable TPA claims processing. With built-in claims editing software that includes over 40 million edits (including CMS NCCI), it actively flags discrepancies and prevents processing errors.
-
Cost-Efficiency: By reducing administrative costs associated with pending claims, Mirra's solution optimizes financial resources for healthcare providers. Built-in fraud, waste, and abuse detection further prevents revenue leakage.
-
Accelerated Turnaround Providers experience expedited payments as Mirra's solution improves the overall turnaround time, expediting claim processing. Payers experience faster resolution with high auto-adjudication rates powered by ClaiMaster®, an EDI claims tool compliant with CMS mandates.
-
Automated Processing: Mirra's healthcare claims adjudication solution seamlessly handles medical, institutional, and dental claims, automating the processing and minimizing the need for manual intervention. It integrates with third-party gateways and supports electronic and paper claims via ClaimsLite® for data entry and ClaiMaster® for EDI processing.
For Providers:
-
Seamless Integration: Mirra's solution integrates smoothly with provider systems, offering tools that support providers' administrative needs and workflows. It enables direct access to pricing, edits, prior authorization, and activity logs from a unified interface.
-
Enhanced Accuracy: The system minimizes errors and improves the accuracy of claims processing, ensuring reliable reimbursement for healthcare providers. High-dollar reviews and built-in quality checks enhance claim integrity from the start.
-
Operational Efficiency: By reducing administrative burdens, Mirra's solution frees up resources and enables providers to focus on delivering quality patient care. Smart queue management and claim categorization simplify back-end operations.
-
Faster Payments: Providers experience expedited payments as Mirra's solution improves the overall claims processing time, enhancing cash flow. Real-time dashboards and claim tracking further contribute to a smoother revenue cycle.
-
Streamlined Workflow: Mirra's automated processing capabilities reduce manual tasks and improve efficiency across the claims adjudication process for providers. Features like global search, document uploads, and instant access to service/provider details streamline day-to-day tasks.

Mirra’s Claims Adjudication Solution’s Advanced Features at a Glance
-
Account Management: View client AR ledgers, claim details, service information, provider details, edits, documents, notes, maximum out-of-pocket (MOOP), activity logs, and more.
-
File and Queue Management: Effortlessly manage files, upload various documents, encounter files, and categorize TPA claims into specific queues for streamlined processing.
-
Comprehensive Reporting: Access SSRS/Power BI reports and scheduled reports, providing valuable insights into healthcare claims management and processing.
-
Member and User Management: Easily search and manage members, handle prior authorizations, generate various letters such as explanations of benefits/payments, rejected letters, and more.
Recent industry stats reflect a 5-15% annual surge in claim denials, necessitating innovative, automated solutions for streamlined and error-free claims adjudication.
Also, read Optimize Revenue with Advanced Claims Adjudication
Why Choose Mirra's Claims Adjudication Solution?
When we talk about Mirra's solution, it stands out because it offers an ideal platform for different plan types, ensuring a high auto-adjudication rate and significantly improving the quality and timeliness of claims processing. Implementing Mirra's Automated Claims Adjudication Solution significantly alleviates the operational burden on healthcare staff, substantially enhancing productivity.
Heightened Productivity
The solution effectively tackles laborious administrative tasks through streamlined automation, allowing staff to concentrate on more critical aspects of healthcare provision. Integrating Mirra's solution has improved staff efficiency by minimizing time-consuming manual processes. This shift has led to a notable increase in staff productivity, ensuring their focus remains on delivering quality care instead of administrative complexities.
Enhanced Resource Management
The implementation of Mirra's solution optimizes resource allocation within healthcare facilities. By automating numerous administrative functions effectively, staff can dedicate more time to patient-centric activities, enhancing the overall quality of healthcare services.
Realizing Operational Efficiency
Adopting Mirra's Automated Claims Adjudication Solution results in streamlined operations, enabling healthcare providers to channel their resources more effectively towards delivering superior patient care management services. The optimization of staff efforts facilitates a more patient-centric approach while maintaining operational efficiency in the healthcare ecosystem.
Read more: 7 Benefits of Outsourcing your Medical Claims Management | Mirra HC
Financial Implications and Revenue Enhancement with Mirra's Solution

The implementation of Mirra's Automated Claims Adjudication Solution not only optimizes operational workflows but also yields financial benefits for healthcare providers. The system's precision in processing claims and its reduced error rates significantly impact the economic landscape within healthcare organizations.
Enhanced Cost Efficiency
Mirra healthcare’s Claims Adjudication solution minimizes operational costs related to claims processing. Reducing manual interventions and streamlining operations mitigates the overhead expenses associated with error corrections, rework, and long processing times. This efficiency boost translates into essential cost savings for healthcare providers, enhancing their financial health.
Also, read Explore How Claims Adjudication Can Control Healthcare Costs
Revenue Acceleration
Automation improves the claims adjudication process with fewer pending claims and a faster turnaround time, Mirra's solution accelerates revenue cycles for healthcare providers. More secured claims approvals mean quicker reimbursement, positively impacting cash flow and overall revenue generation.
Improved Return on Investment (ROI)
The implementation of Mirra's solution represents a significant return on investment. Reducing administrative costs and increased efficiency and accuracy in claims processing results in an impressive ROI for healthcare organizations. Moreover, the solution's smooth integration minimizes additional technology-related expenses, augmenting its overall financial benefits.
Concrete Financial Gains
Mirra's Automated Claims Adjudication Solution offers a tangible impact on the financial front. Through its cost efficiencies, accelerated revenue cycles, and substantial ROI, healthcare providers significantly improve their financial standing, reinforcing the value proposition of Mirra's automation within the healthcare ecosystem.
Read more: 5 Solutions to Bring Down Your Claims Denial Rate | Mirra HC
Enhancing Patient Experience Through Mirra's Automation

The following are some ways in which Mirra's claims adjudication solution enhances patient experience:
-
Enhanced Information Accuracy: Ensures precise patient data management, minimizing errors and ensuring consistent, reliable information across all touchpoints. Improves personalization and tailoring of healthcare services.
-
Empowering Patient Engagement: Facilitates proactive communication, providing automated updates on claim status, billing, and appointments. Empowering patients with timely information fosters involvement and trust in their healthcare journey.
-
Streamlined Administrative Processes: It increases efficiency, reducing wait times and expediting service delivery. Automation allows stakeholders to focus on quality care, ensuring quicker responses and minimizing administrative bottlenecks.
The Bottom Line
Mirra's Claims Adjudication Solution is a versatile and transformative tool that optimizes the claims adjudication process for both payers and providers. By leveraging automation, Mirra Health Care empowers healthcare organizations to streamline operations, reduce errors, and enhance financial performance. With smart automation, seamless integration, and powerful reporting, Mirra makes the entire claims process faster, more accurate, and cost-effective. It also lightens the administrative load so teams can focus more on delivering care and less on paperwork.
Whether you are a payer or a provider, Mirra's customized solution delivers accuracy, efficiency, and cost savings to support your healthcare journey. Reach out to us for a custom demo.