For health plans, navigating the complexities of Medicare billing services can feel like an uphill task. Manual processes, retroactivity intricacies, and delayed payments create inefficiencies, erode profitability, and strain member relationships. But what if we could help you turn things around?
This blog post will discuss key challenges in TPA premium billing and offer actionable strategies that can empower you to automate workflows, master retroactivity, optimize payments, prioritize transparency, and leverage data insights. Let's get started.
Key Challenges in Medicare Advantage Premium Billing Systems
Let's look at the major challenges in Medicare Advantage Premium Billing systems:
1. Data Accuracy Challenges: Manual data entry, despite its prevalence, causes errors at a significant rate, approximately 5%. This results in considerable financial losses and dissatisfaction among members.
2. Retroactivity Management Complexity: Handling complex adjustments, prorated charges, and varying effective dates poses a significant challenge. Manual calculations are prone to errors and are time-consuming, potentially resulting in financial discrepancies and member dissatisfaction.
3. Payment Delays: Late payments disrupt cash flow, strain resources, and affect plan stability. Traditional payment processing methods are often slow and inconvenient, while manual reminders and follow-up calls consume valuable staff time. These delays have a ripple effect, impeding financial health and operational efficiency.
4. Transparency Issues: Opacity in billing statements and infrequent communication contribute to member frustration and payment delays. Without clear explanations and timely updates, members navigate a confusing billing environment, potentially eroding trust and leading to delayed payments.
5. Integration Challenges: Managing disparate systems for billing, member portals, and claims management leads to data silos and operational inefficiencies. Manual data transfer is error-prone, necessitates constant reconciliation, and hampers accuracy and efficiency.
These challenges are not mere inconveniences but strategic impediments to financial sustainability and member satisfaction. However, there's an innovative solution to the problem: Mirra Health Care's TPA Premium Billing system, which helps streamline workflows and enhance operational efficiency.
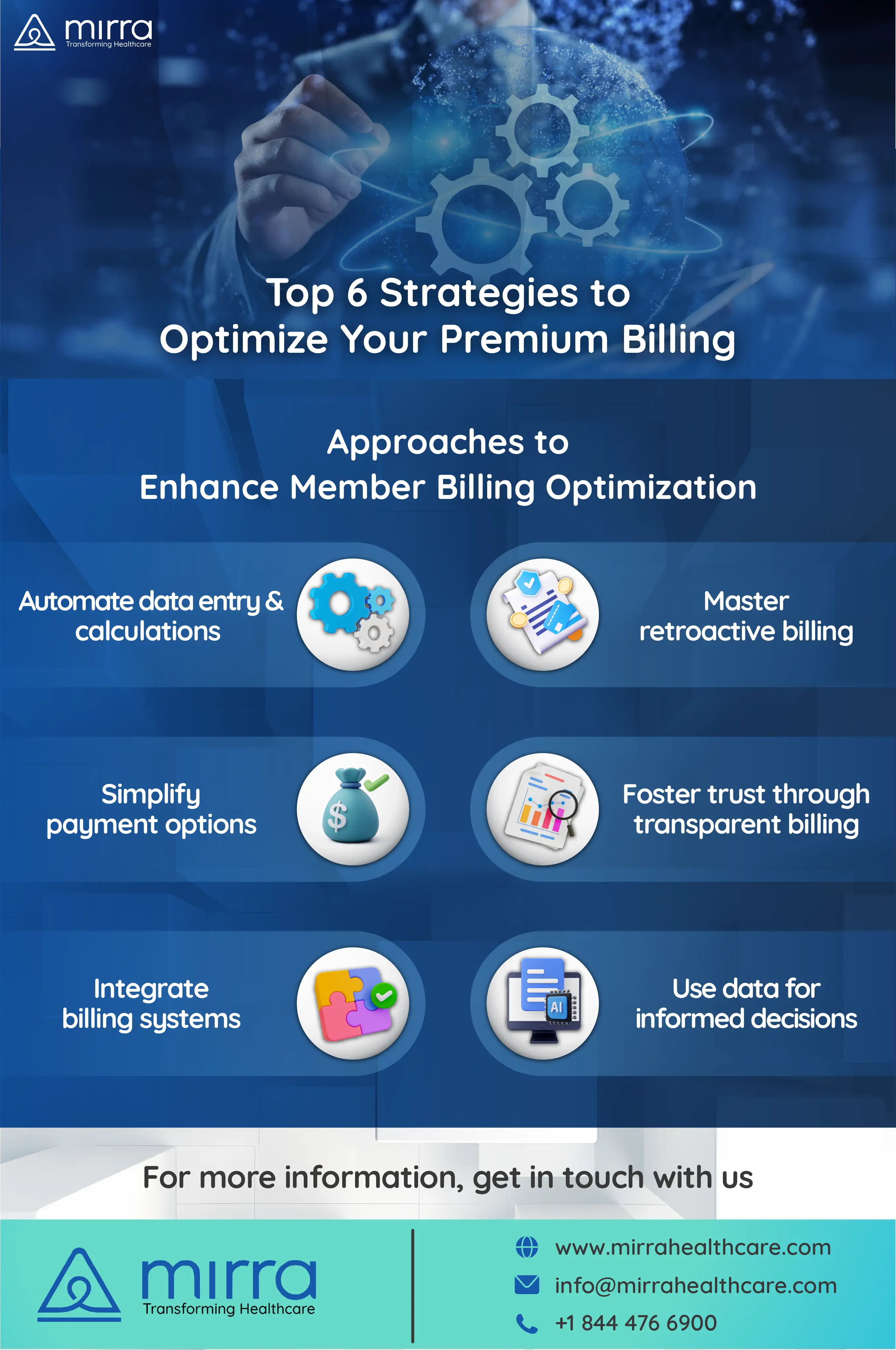
Strategies for Optimized Premium Billing
With the challenges outlined, let's explore actionable strategies to transform your premium billing system into a well-oiled machine:

Embrace Automation
Ditch the error-prone world of manual data entry. Implement software automating data import, calculations, and adjustments, slashing error rates by up to 80%, as reported by industry studies. Imagine the time and resources saved, free to focus on strategic initiatives.
Conquer Retroactivity with Confidence
Complex adjustments and prorated charges are no longer nightmares. Leverage robust software designed to handle intricate retroactivity rules, ensuring accurate calculations and eliminating discrepancies. This translates to improved financial forecasting and satisfied members.
Streamline Payments, Boost Collections
Offer diverse payment options like, credit cards, debit cards, etc., and support SSA withholding for payments. Utilize automated reminders and follow-up mechanisms to reduce late payments and boost collection rates by an average of 15%, as shown by industry benchmarks.
Transparency The Key to Building Trust
Empower members with clear, concise invoices. Leverage software features that provide detailed explanations of charges and offer self-service options, fostering trust and reducing inquiries.
Break Down Silos, Integrate Seamlessly
Eliminate data silos and streamline workflows by integrating your billing system with claims management and other vital software. This ensures data accuracy, improves efficiency, and eliminates the need for manual data transfer.
Leverage Data Insights for Smarter Decisions
Gain valuable insights through comprehensive reporting features. Identify trends, analyze member behavior, and optimize billing processes based on data-driven decisions. This proactive approach fosters continuous improvement and drives financial sustainability.
These strategies are building blocks for a holistic transformation. By leveraging the power of Mirra’s Premium Billing software, you can conquer challenges, optimize efficiency, and unlock the true potential of your revenue cycle.
Streamline Your Premium Billing with Mirra Health Care
Mirra Health Care's Premium Billing solution can help you transform your member billing ecosystem. Here's what sets us apart:
Effortless Automation
- Say goodbye to manual data entry: Generate invoices and post payments automatically, saving you significant time and reducing errors.
- Conquer retroactivity with ease: Our system seamlessly handles intricate adjustments and CMS regulations, ensuring accuracy and financial predictability.
- Simplify member management: Mirra’s premium billing system is fully integrated with our Enrollment or Membership system for effortless data synchronization and streamlined operations.
Unmatched Accuracy
- Eliminate data discrepancies: Reduce errors and ensure financial transparency with our robust system and automated processes.
- Gain complete visibility: Track and reconcile various payment sources easily, from LIS and SSA payments to member contributions.
- Boost member satisfaction: Clear and accurate invoices foster trust and confidence, reducing inquiries and improving communication.
Enhanced Efficiency
- Spend less time on administrative tasks: Free up your team to focus on strategic initiatives with our intuitive and user-friendly interface.
- Streamline workflows: Automate repetitive tasks and eliminate manual data transfer for improved operational efficiency.
- Make data-driven decisions: Leverage valuable insights and reports to optimize billing processes and identify growth opportunities.
Beyond Features, a Partnership
We understand your unique needs. That's why we offer:
- Dedicated implementation specialists for a smooth transition and rapid value realization.
- Ongoing support and training to empower your team and maximize the solution's potential.
- A commitment to innovation to keep you ahead of the curve with cutting-edge features and industry expertise.
The Bottom Line
Ready to experience the difference? Contact us today for a personalized no-obligation demo and see how Mirra Health Care, a leading third-party administrator in Florida can help you. Don't settle for the ordinary. Partner with Mirra Health Care’s Medicare Advantage in a Box and unlock the extraordinary potential of your premium billing. Contact us now.